У свету медицинских набавки, мало је ствари које су тако фундаменталне, али тако сложене као лице маска. Од једноставног хируршка маска на високо специјализовану N95 респиратор, разумевање нијанси се не односи само на поштовање – ради се о заштити живота. Као менаџер набавке, ви сте на првој линији набавке, а одлуке које доносите имају директан утицај на пацијенте и здравствене заштите професионалци. Овај водич је за вас. Као Ален, произвођач са више од деценије искуства у производњи медицинског потрошног материјала за једнократну употребу за глобална тржишта као што су САД и Европа, желим да пресечем забуну. Истражићемо другачије врсте маски, декодирајте прописе и пружите практичне увиде који ће вам помоћи да поуздано пронађете извор. Ово није само још један чланак; то је поглед иза завесе из фабричке перспективе, дизајниран да одговори на ваша најхитнија питања.
Која је права разлика између хируршке маске и Н95 респиратора?
На први поглед, а хируршка маска и ан N95 респиратор може изгледати слично, али њихове функције, дизајн и намена су различити. А хируршка маска је лабавог кроја, за једнократну употребу уређај који ствара а физичка баријера између уста и носа носилац и потенцијалних загађивача у непосредном окружењу. Његова примарна сврха је блокирање великих честица капљица трансмисије, попут прскања или спреја, штитећи друге од респираторних емисија носиоца. Израђују се хируршке маске од нетканог материјала и често се користе у стерилним срединама током медицинских процедура да заштити оба пацијента и здравствени радник из пренос микроорганизама, телесне течности, и честица материјала. Међутим, због лабавог кроја, често постоји а јаз између ивице маске и лице, што значи да не нуди потпуну заштиту од удисања мањих ваздушним честице.
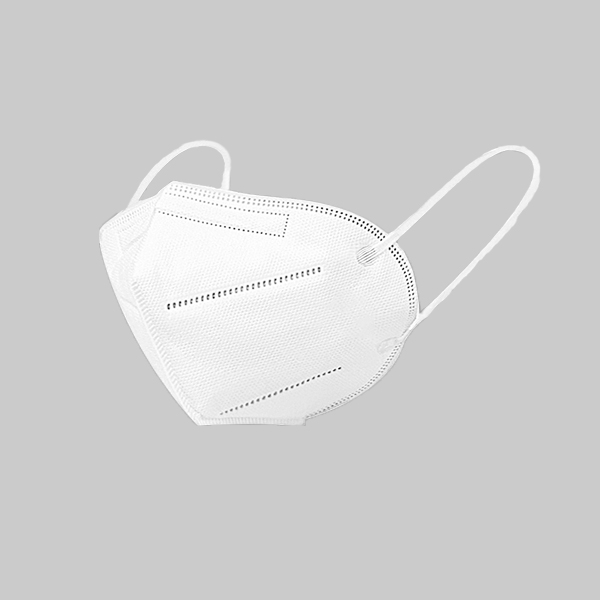
Ан N95 респиратор, с друге стране, је а респираторни заштитни уређај дизајниран да постигне веома блиско пристајање лица и веома ефикасан филтрација оф ваздушним честице. Ознака "Н95" значи да када се подвргне пажљивом тестирању, респиратор блокира најмање 95 процената веома малих (0,3 микрона) тест честица. Ово чини N95 респиратор ефикасан против великих и малих честица. За разлику од а хируршка маска, ан N95 респиратор је дизајниран тако да се чврсто залепи за лице, присиљавајући удахнути и издахнути ваздух да прође кроз њега филтер материјала. Ово чврсто заптивање је кључно за његову ефикасност. Због тога се сматра личном заштитном опремом (ППЕ) намењен да користи за заштиту тхе носилац од излагања штетним честицама у ваздуху.
Поједностављено речено, а хируршка маска штити животну средину из тхе носилац, док је ан N95 респиратор штити носилац из животне средине. Као менаџер набавке, разумевање ове разлике је први корак у обезбеђивању да ваш објекат буде снабдевен правом врстом маска за прави задатак. Не бисте користили једноставну процедуру маска током поступка стварања аеросола, и не би вам требао скуп N95 за посетиоца који иде ходником. Прави избор оптимизује безбедност и ефикасно управља трошковима.
Како су медицинске маске регулисане у различитим здравственим установама?
Регулатива о медицинске маске је критичан аспект који директно утиче на безбедност пацијената и лекара и значајно варира у зависности од врсте маска анд тхе постављање. У У.С., Управа за храну и лекове (ФДА) и Национални институт за безбедност и здравље на раду (НИОСХ), део CDC, су примарна тела која регулисати ови производи. То је двоструки систем који може бити збуњујући, али осигурава да сваки маска испуњава специфичне стандарде перформанси за своју предвиђену употребу. За професионалце у области набавке, ово није само бирокрација; то је ваша гаранција квалитета и безбедности.
Хируршке маске, на пример, регулисани су ФДА као медицинска средства ИИ класе. Морају испунити посебне захтеве за заштита баријере течности и филтрација ефикасност. Тхе ФДА‘с пропис под 21 ЦФР 878.4040 наводи стандарде за ове маске за медицинске процедуре. Тестирани су за ствари као што су ефикасност бактеријске филтрације (БФЕ), ефикасност филтрације честица (ПФЕ), отпорност на течност и запаљивост. Ово осигурава да маска може да издржи прскање крви или других инфективних материјала током процедуре. А маска односно Одобрено од стране ФДА пружа вам поверење да је прегледан за безбедност и ефикасност за употребу у а здравствено окружење. Ово су типови стандарда 3-слојне медицинске маске за лице за једнократну употребу са омчама за уши који су неопходни за општу негу пацијената и контролу инфекције.
Респиратори са филтером за лице (ФФР), као нпр Н95с, другачије су регулисане. Ако су намењени за општу индустријску употребу (као грађевинарство), надгледају их НИОСХ под 42 ЦФР део 84. НИОСХ тестира и потврђује да ови респиратори испуњавају минималне стандарде филтрације и конструкције. Међутим, када је ан N95 респиратор је намењен за употребу у а здравствено окружење за заштиту од патогена који се преносе ваздухом, мора испуњавати захтеве за обоје НИОСХ анд тхе ФДА. Ови уређаји са двоструким сертификатом су познати као хируршки Н95 респиратори. Они пружају респираторну заштиту N95 и заштита од баријере течности а хируршка маска.
Можете ли објаснити улоге НИОСХ-а и ФДА у одобравању маски?
Разумевање различитих улога НИОСХ анд тхе ФДА је најважније за сваког менаџера набавке који набавља заштиту за дисање. Замислите их као два различита стручњака који осигуравају да је производ безбедан и ефикасан из два различита угла. Национални институт за Безбедност и здравље на раду (НИОСХ) је истраживачка агенција фокусирана на безбедност радника. Његова примарна улога у вези са респираторима је да тестира и потврди да испуњавају строгу конструкцију, филтрација, и стандарди перформанси. Када видите а НИОСХ одобрење на ан N95 респиратор, то значи да је маска је ригорозно тестиран како би се осигурало да филтрира најмање 95% немасних честица у ваздуху. Ова сертификација се односи на заштиту радника—у овом случају, здравствене заштите професионалним.
Управа за храну и лекове (ФДА), с друге стране, регулише медицинске маске и уређаје који осигуравају да су безбедни и ефикасни за јавно здравље. За а хируршка маска или а хируршки респиратор Н95, тхе ФДАЊен интерес је да се користи као медицинско средство. Тхе ФДА прегледа ове производе преко а обавештење пре тржишта [510(к)] поднесак да се утврди да ли су безбедни за употребу у медицини подешавања неге. Тхе ФДАКлиренс се фокусира на својства као што су отпорност на течност, биокомпатибилност (обезбеђујући да материјали неће иритирати кожу) и запаљивост. Тхе ФДАУлога је да регулисати тхе маска као баријера за заштиту од прскања, прскања и капљица великих честица, што је критично током хируршке процедуре за заштиту и пацијента и пружаоца.
Дакле, да резимирамо:
- НИОСХ потврђује респираторспособност да филтер честице у ваздуху за заштиту носилац.
- ФДА чисти а хируршка маска или хируршки респиратор Н95 за његову употребу као медицински уређај, фокусирајући се на његову способност да делује као а течна баријера.
Стандардна индустријска N95 респиратор само потребе НИОСХ одобрење. Али а хируршки респиратор Н95 потребе обоје НИОСХ одобрење за његове могућности филтрације и ФДА одобрење за његову употребу као хируршки уређај отпоран на течност. Као купац, ако вам треба а респиратор за операциону салу или друга подешавања са ризиком од излагања течности, морате потражити а маска који има обе акредитиве.

Зашто је правилно пристајање тако критично за Н95 респиратор?
Ан N95 респиратор је ефикасан само колико и његов печат. Док је филтер медиј је дизајниран да блокира најмање 95% честица, овај високи ниво заштите је потпуно нарушен ако ваздух може да цури око ивице маске. Ово је једина најважнија разлика између а респиратор и стандард маска за лице. А хируршка маска лабаво прекрива лице, али ан N95 респиратор је пројектован за а блиско пристајање лица. Без овог чврстог заптивања, контаминирани ваздух ће пратити пут најмањег отпора, заобилазећи филтер и улазак у зону дисања корисника кроз јаз. Ово негира саму сврху ношења високе филтрације респиратор.
Постизање а правилно пристајање укључује неколико корака. Прво, респиратор мора бити одговарајуће величине и облика за лице корисника. Нису сва лица иста, због чега многи произвођачи нуде различите моделе и величине. Друго, тхе носилац морају бити обучени како да се правилно облаче и скидају маска. Ово укључује савијање наставка за нос како би се прилагодио мосту нос и уста области и уверите се да су траке правилно постављене. Коначно, за професионалне користити у У.С., ОСХА захтева од радника да прођу тест способности. Ово је формална процедура која проверава цурење око заптивке. Фактори попут длаке на лицу може да омета заптивање, чинећи тест уклапања немогућим и отежавајући респиратор неефикасна.
Као менаџер набавке, ваша одговорност се протеже даље од саме куповине Н95с. Ради се о томе да ваша организација има свеобухватан програм заштите респираторних органа. То значи пружање различитих респиратор модели за прилагођавање различитих структура лица и подржавање неопходне обуке и протокола за тестирање фит. Јефтино N95 респиратор то никоме не одговара није погодба; то је обавеза. Комуникација са вашим добављачем о различитим величинама и облицима које они нуде је кључни део информисане куповине. Поуздан произвођач би требало да буде у могућности да пружи детаљне спецификације и подржи програм тестирања вашег објекта.
Шта су хируршки Н95 респиратори и када су потребни?
A Хируршки респиратор Н95 је хибридни шампион медицинске маске, нудећи највиши ниво заштите у захтевним здравствене установе. Комбинује карактеристике стандарда N95 респиратор са онима од а хируршка маска. То значи да не само да пружа НИОСХ одобрену респираторну заштиту од честица у ваздуху, већ такође Одобрено од стране ФДА као а Класа ИИ медицински производ због његове отпорности на продирање течности. Замислите то као ан N95 носећи кабаницу. Дизајниран је да заштити оба пацијента и здравствени радник (ХЦП) током процедура где постоји висок ризик од патогена у ваздуху и прскања или прскања крви и телесне течности.
Ови респиратори двоструке намене су посебно намењен за употребу у срединама где су стерилност и заштита од ваздуха и течности најважнији. Ово укључује операционе сале, одељења за хитне случајеве током неге трауме и током процедура које стварају аеросол код пацијената са познатим или сумњивим заразним болестима, као што су интубација или бронхоскопија. Тхе ширење ЦОВИД-19 донео је важност Хируршки Н95 у оштар фокус, јер је нудио свеобухватну заштиту од вируса који се преноси путем капљица и аеросола. Тхе баријера течности или ефикасност филтрације ових маски је ригорозно тестиран како би се осигурало да пружају поуздан штит.
Приликом набавке, кључно је потврдити да а маска на тржишту као "Хируршки Н95“ је истински сертификован од стране оба НИОСХ анд тхе ФДА. Требало би да будете у могућности да пронађете а НИОСХ број одобрења на респиратор себе (нпр. ТЦ-84А-кккк) и потврдите да га је обрисао ФДА под шифра производа МСХ. Не може се преговарати о раду са транспарентним добављачем који може да обезбеди ову документацију без оклевања. Иако су ови респиратори скупљи, они су неопходан део ППЕ у високоризичном подешавања неге, а компромис у погледу њиховог квалитета није опција.
Да ли вентили за издисање на респиратору угрожавају безбедност у клиничком окружењу?
Вентили за издисање на а респиратор су карактеристика дизајнирана за удобност, али имају значајне импликације за употребу у а здравствено окружење. А вентил је једносмерни поклопац који се отвара када се носилац издише, омогућавајући топлом, влажном ваздуху да лако изађе. Ово чини респиратор удобније за ношење током дужег периода и смањује накупљање топлоте у унутрашњости маска. За индустријске раднике, попут оних у грађевинарству или производњи, ово је фантастична карактеристика. Међутим, у медицинском контексту, посебно за контролу извора, то исто вентил постаје велики проблем.
Питање је у томе што вентил за издисање омогућава да се нефилтриране респираторне капљице носиоца избаце директно у околину. Док је вентил не угрожава заштиту особе која носи респиратор, потпуно негира сврху маске у спречавању носилац од ширења клица на друге. У стерилном пољу или када се бринете о имунокомпромитованим пацијентима, ово је неприхватљив ризик. Током COVID-19 пандемија, CDC изричито се препоручује против употребе респиратора са вентили за издисање за контролу извора, јер они мало раде помоћи у смањењу ширење вируса од заражене особе.
Стога, за скоро све здравствене установе, респиратори са вентили за издисање нису прикладне. Када ти носити лице маска у болници или клиници, циљ је двострук: заштитите себе и заштитите оне око себе. А вентилирани респиратор постиже само први циљ. Као менаџер набавке, ово је критичан детаљ на који треба обратити пажњу. Осим ако не купујете за врло специфичну професионалне задатак где контрола извора није проблем (што је реткост у здравствене заштите), увек треба да се одлучите за Н95с или друге респираторе без a вентил. Ово осигурава да пружате боља заштита за целокупно окружење за негу.

Шта треба да тражим када набављам медицинске маске из иностранства?
Соурцинг медицинске маске од произвођача у земљи као што је Кина може бити веома повољан у смислу трошкова и обима, али захтева марљивост и јасну стратегију. Као власник фабрике, сваки дан разговарам са менаџерима набавке као што сте ви, и знам вашу забринутост. Кључ је да се превазиђе цена и фокусира се на партнерство и верификацију. Прво и најважније, захтевајте транспарентност у документацији. Реномирани произвођач ће вам спремно доставити свој ИСО 13485 сертификат (за системе управљања квалитетом медицинских уређаја), документацију са ЦЕ ознаком (за европска тржишта) и све релевантне ФДА писма о регистрацији или одобрењу. Не верујте им само на реч; затражите документе и знате како да их оверите.
Друго, комуникација је све. Једна од највећих болних тачака за које чујем је неефикасна комуникација. Потребан вам је добављач са тимом за продају и подршку који говори енглески језик и разуме ваше техничке и регулаторне захтеве. Поставите им детаљна питања о њиховом производном процесу, контроли квалитета и системима праћења серија. Да ли вам могу рећи која је количина сировина ушла у маска купујеш? Добар партнер може. Овај ниво детаља је такође кључан за логистичко планирање. Разговарајте о времену испоруке, опцијама испоруке и условима плаћања унапред да бисте избегли кашњења због којих би ваш објекат могао да остане без залиха.
На крају, размотрите сам производ. Затражите узорке пре него што наручите велику наруџбу. Када их добијете, пажљиво проверите квалитет. Проверите заварене спојеве на ушне петље, осећај за прозрачна тканина, и интегритет наставка за нос. Упоредите то са а маска знаш и верујеш. Да ли се осећа слабо? Има ли чудних мириса? Ови мали детаљи могу бити показатељи већих проблема у контроли квалитета. Набавка из иностранства подразумева изградњу поверења. То је партнерство у којем обе стране имају користи од јасноће, квалитета и отворене комуникације. Било да тражите висококвалитетне изолационе хаљине или једноставан маска за лице, ови принципи дужне пажње увек важе.
Како је пандемија ЦОВИД-19 променила пејзаж маски за лице?
Тхе COVID-19 пандемија је била сеизмички догађај који је суштински преобликовао глобално разумевање и употребу маска за лице. Пре 2020, у многим западним земљама, маска-ношење је углавном било ограничено на здравствене установе. Пандемија је трансформисала маска у свеприсутни симбол јавног здравља и друштвене одговорности, који носе општој јавности дневно. Ова потражња без преседана створила је огромну кризу глобалног ланца снабдевања, разоткривајући рањивости и доводећи до пораста нове производње, како легитимне тако и лажне. За професионалце у области набавке, тржиште је постало хаотичан пејзаж нових акронима (КН95, ФФП2), непроверени добављачи и фалсификовани производи.
Један од најзначајнијих померања био је фокус на контролу извора. Примарна порука јавног здравља постала је да ношење а маска није се радило само о заштити личности, већ о заштити заједнице. Ово је подигло важност чак и једноставног платнена маска или поступак маска у смањењу ширење ЦОВИД-19. Тхе CDC и друге здравствене агенције издале су детаљна упутства како да носити лице ефикасно покривање, укључујући препоруке за побољшати пристајање хируршких и платнене маске везивањем ушних петљи или употребом монтажера маски. Пандемија је демократизовала маска, али је и створило знање јаз због чега су многи потрошачи, па чак и неки професионалци, били збуњени различите врсте маски.
Из перспективе производње и набавке, пандемија је изазвала брзу еволуцију. Видели смо одобрења за хитну употребу (ЕУА) од ФДА како би се омогућила употреба нетрадиционалних респиратора, попут КН95 из Кине, у здравствене заштите подешавања када Н95с били оскудни. Ово је нагласило важност разумевања међународних стандарда. Такође је подвучена критична потреба за робусном верификацијом ланца снабдевања. Криза нас је научила да је ослањање на један извор или регион ризично и да је успостављање односа са поузданим, сертификованим произвођачима непроцењиво. Наслеђе од COVID-19 је тржиште које је свесније, проницљивије и захтевније за квалитет и транспарентност у свом ППЕ.
Да ли су платнене маске или маске за стандардне процедуре погодне за здравствену заштиту?
Погодност а платнена маска или стандардном процедуром маска у потпуности зависи од конкретног задатка и нивоа ризика у оквиру здравствено окружење. А платнена маска је првенствено уређај за контролу извора за општој јавности. Док је а добро пристаје платнена маска може помоћи у смањењу емисија респираторних капљица из носилац, нуди минималну заштиту носилац од удисања финих честица или аеросола. Из тог разлога, платнене маске се генерално сматрају неадекватним за клиничку употребу од стране здравствених радника који пружају негу пацијентима. Недостају им строги филтрација и стандарди отпорности на течност који се захтевају од медицинске маске.
Стандардна процедура медицинске маске, који су врста хируршка маска, су друга прича. Они су главни у здравствене заштите. Ове за једнократну употребу маске су Регулисано ФДА и дизајниран да обезбеди баријеру против капљица и прскања. Савршено су погодни за широк спектар задатака, као што су општи прегледи, транспорт пацијената и употреба у заједничким просторијама болнице за промовисање контроле извора. Нуде добар баланс заштите и прозрачности за ситуације ниског ризика. Међутим, они су не a респиратор. Не формирају чврсто заптивање и не пружају поуздану заштиту од удисања малих патогена у ваздуху.
Стога је основно правило да се подудара са маска на ризик.
- Маска од тканине: Није за клиничку употребу од стране здравствених радника.
- Процедура/хируршка маска: Идеалан за контролу извора и заштиту од капљица у клиничким ситуацијама ниског ризика. Неопходан за заштиту пацијената од испуштања провајдера током стерилних процедура.
- N95 респиратор: Потребан за заштиту од честица у ваздуху, посебно током поступака стварања аеросола.
За менаџера набавке, ово значи одржавање вишеслојног инвентара. Треба вам поуздано снабдевање високог квалитета медицинске хируршке маске за лице за свакодневну употребу, заједно са залихама од НИОСХ-одобрено Н95 респиратори за сценарије високог ризика. Ради се о томе да имате прави алат за посао који треба да осигурате усклађеност и безбедност.
Навигација по сертификатима: Шта ИСО, ЦЕ и ФДА заиста значе за вашу куповину маске?
За менаџера набавке, сертификати су ваш језик од поверења. Они су објективни доказ да производ испуњава утврђене стандарде. Хајде да разложимо оне најчешће на које ћете се сусрести приликом проналажења извора медицинске маске.
ИСО 13485 је међународни стандард за систем управљања квалитетом за производњу медицинских уређаја. Када је фабрика попут моје сертификована по ИСО 13485, то значи да смо показали своју способност да обезбедимо медицинске уређаје који доследно испуњавају захтеве купаца и применљиве регулаторне захтеве. То није сертификат производа; то је сертификација процеса. То вам говори да произвођач има снажне системе за пројектовање, производњу, следљивост и управљање ризиком. Ово је ваша основна гаранција у компетентност и поузданост добављача за све производе, од маска за лице на сложеније предмете као што су медицинске усисне спојне цеви.
ЦЕ ознака је сертификациони знак који указује на усаглашеност са стандардима здравља, безбедности и заштите животне средине за производе који се продају у Европском економском простору (ЕЕА). За а хируршка маска или респиратор, ЦЕ ознака означава да је производ процењен да испуњава релевантне директиве или прописе ЕУ (као што је Уредба о медицинским уређајима или Уредба о личној заштитној опреми). То је обавезан пасош за производе који улазе на тржиште ЕУ. За купца са седиштем у САД, иако није директан захтев, он служи као снажан показатељ да се произвођач придржава високих међународних стандарда.
Коначно, ФДА (Управа за храну и лекове) регулише медицинске маске у Сједињеним Државама. Као што смо разговарали, хируршке маске сматрају се Класа ИИ медицинска средства и захтевају ФДА одобрење, обично кроз 510(к) обавештење пре тржишта. Овај процес показује да је уређај барем једнако безбедан и ефикасан као и легално продати уређај који не подлеже одобрењу пре тржишта. За Хируршки респиратори Н95, захтевају обоје НИОСХ одобрење и ФДА клиренс. Верификација добављача ФДА регистрација и царињење производа су корак о којем се не може преговарати у вашем процесу дужне пажње. Поуздани добављач ће на захтев обезбедити своје регистрационе бројеве и 510(к) одобрења. Ови сертификати су ваш штит од лошег квалитета и неусаглашености са прописима.
| Феатуре | Хируршка маска | Н95 респиратор (индустријски) | Хируршки респиратор Н95 |
|---|---|---|---|
| Примари Пурпосе | Баријера за течност, контрола извора | Филтрација честица за корисника | И баријера течности и филтрација |
| Фит | Лоосе-фиттинг | Заптивка која добро пријања | Заптивка која добро пријања |
| Филтрација | Блокира велике капљице | Филтрира ≥95% честица у ваздуху | Филтрира ≥95% честица у ваздуху |
| Цурење | Високо цурење око ивица | Мало цурење када је тестирано | Мало цурење када је тестирано |
| Уредба САД | ФДА (21 ЦФР 878.4040) | НИОСХ (42 ЦФР, део 84) | НИОСХ и ФДА |
| Отпорност на течност | Да (тестирао од АСТМ методе) | бр | Да (ФДА одобрено) |
| Случај употребе | Општа брига о пацијентима, хирургија | Грађевинарство, производња | Поступци стварања аеросола |
Кључне ствари које треба запамтити
Док се крећете по сложеном свету медицине маска и респиратор набавке, имајте на уму ове битне тачке:
- Функција диктира форму: A хируршка маска штити друге из тхе носилац блокирањем капљица. Ан N95 респиратор штити носилац из животне средине филтрирањем честица у ваздуху.
- Фит је све за респиратор: Ан N95 респиратор је неефикасан без чврстог заптивања. А правилно пристајање, потврђен тестом уклапања, кључан је за постизање обећаног нивоа заштите.
- Упознајте своје регулаторе: У САД, ФДА регулише хируршке маске као медицинска средства, док НИОСХ потврђује перформансе филтрације респиратора. Хируршки Н95с морају задовољити стандарде оба.
- Вентили су за удобност, а не за клинику: Респиратори са вентили за издисање заштитити носилац али не и оне око њих. Они су углавном неприкладни за здравствене установе где је контрола извора витална.
- Провери, не веруј: Када набављате на међународном тржишту, захтевајте и верификујте сертификате као што су ИСО 13485, ЦЕ ознаке и ФДА клиренс. Партнер са транспарентним добављачима који дају приоритет квалитету и комуникацији.
- Ускладите маску са ризиком: Користите вишестепени приступ. Стандард залиха медицинске маске за општу употребу и резерву Н95 респиратори за високоризичне процедуре које стварају аеросол како би се осигурала сигурност и ефикасно управљање трошковима.
Пост тиме: Јул-23-2025





